Staff Reporter:
Due to declining spending in maternal and newborn health, global progress in lowering the early mortal-ity of pregnant women, mothers, and babies has stagnated for eight years, a new UN World Health Or-ganization (WHO) report said.
The report, titled “Improving maternal and newborn health and survival and reducing stillbirth,” analyz-es the most recent statistics, which share similar risk factors and causes, and tracks the provision of criti-cal health services.
The new publication was launched at a major global conference in Cape Town, South Africa.
Overall, the analysis demonstrates that improvements in survival have stalled since 2015, as evidenced by the annual average of 290,000 maternal fatalities, 1.9 million stillbirths (babies who die after 28 weeks of pregnancy), and a startling 2.3 million infant deaths during the first month of life.
The report shows that over 4.5 million women and babies die every year during pregnancy, childbirth or the first weeks after birth, equivalent to one death happening every seven seconds. Most of the deaths were from preventable or treatable causes if proper care was available.
The COVID-19 pandemic, rising poverty, and worsening humanitarian crises have intensified pressures on stretched health systems. Just one in 10 countries (of more than 100 surveyed) report having suffi-cient funds to implement their current plans.
According to the latest WHO survey on the pandemic’s impacts on essential health services, around 25 per cent of countries still report ongoing disruptions to vital pregnancy and postnatal care and services for sick children.
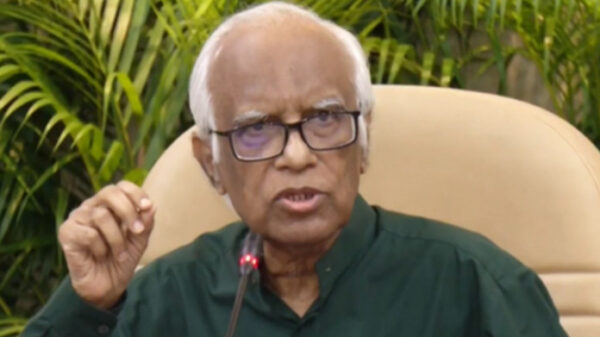
“Pregnant women and newborns continue to die at unacceptably high rates worldwide, and the COVID-19 pandemic has created further setbacks to providing them with the healthcare they need,” said Dr. An-shu Banerjee, Director of Maternal, Newborn, Child and Adolescent Health and Ageing at the World Health Organization (WHO).
“If we wish to see different results, we must do things differently. More and smarter investments in pri-mary healthcare are needed now so that every woman and baby — no matter where they live — has the best chance of health and survival.”
In the worst-affected countries in Sub-Saharan Africa and Central and Southern Asia, the regions with the greatest burden of newborn and maternal deaths, fewer than 60 per cent of women receive even four, of WHO’s recommended eight, antenatal checks.
“The death of any woman or young girl during pregnancy or childbirth is a serious violation of their human rights,” said Dr Julitta Onabanjo, Director of the Technical Division at the United Nations Popu-lation Fund (UNFPA).
“It also reflects the urgent need to scale-up access to quality sexual and reproductive health services as part of universal health coverage and primary health care, especially in communities where maternal mortality rates have stagnated or even risen during recent years. We must take a human rights and gen-der transformative approach to address maternal and newborn mortality, and it is vital that we stamp out the underlying factors which give rise to poor maternal health outcomes like socio-economic inequali-ties, discrimination, poverty, and injustice”.
Based on current trends, more than 60 countries are not set to meet the maternal, newborn, and stillborn mortality reduction targets in the UN Sustainable Development Goals by 2030.